Increased access to better mental health care
SEMPHN commissions services to help address the mental health needs of our community, including people with mild, moderate and severe mental health needs.
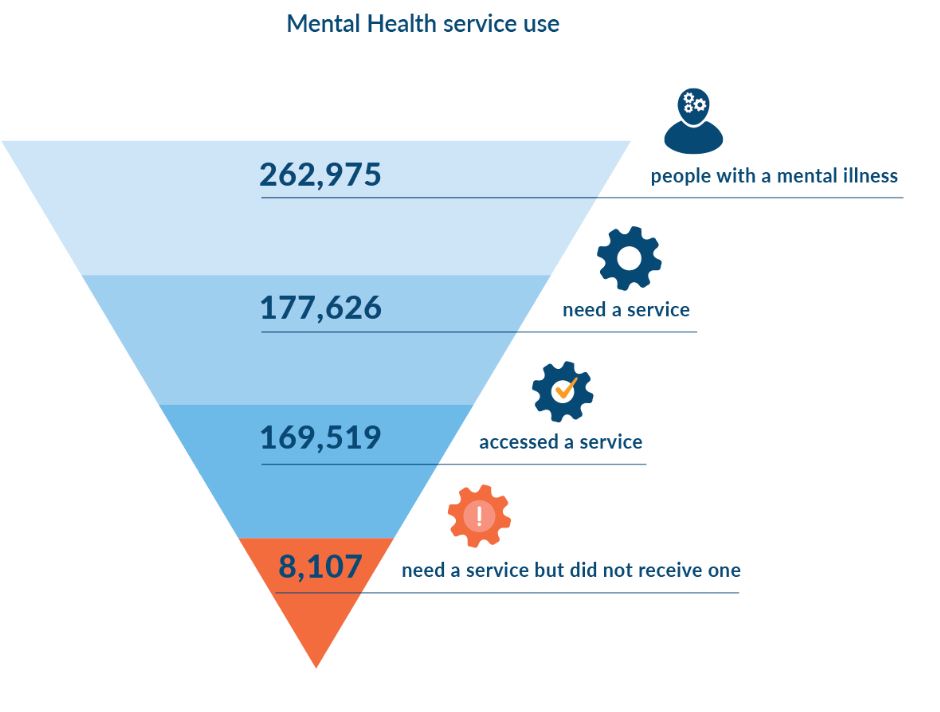
Mental health services we commission range from peer-support, to brief psychological sessions, to individual packages of care. These services form part of our Mental Health Stepped Care Model, which tailors care to individual need and illness severity.
Supporting people with complex needs
Psychosocial Support Services (PSS) aims to address the needs of people with severe mental illness who are not eligible for the National Disability Insurance Scheme (NDIS) to support them to participate in their community and manage day-to-day life activities.
In 2019-20, we commissioned Ermha365 in partnership with Launch Housing to deliver PSS across the region with 450 consumers accessing the service within its first year of service delivery.
PSS provides non-clinical supports that can assist people with severe mental illness to participate in their community, manage daily tasks, undertake work or study, find housing, get involved in activities, and make connections with family and friends. The program empowers and supports people to identify their goals and work towards them.
People can access the following psychosocial support services:
- Psychosocial support sessions
- Group based psychosocial programs
- Assertive outreach and specialist psychosocial Interventions for hard to reach communities
- Support coordination and navigation
- Family and carer psychosocial supports.
Within the past 12 months, Ermha365 and Launch Housing successfully managed and supported the transition of 193 consumers to the Continuity of Support (CoS) program, ensuring continuity of services for these vulnerable consumers.
During COVID-19, PSS continued to support its clients using telehealth and video for individual consultations. Group programs continued to provide virtual activities including online trivia, online peer spaces, self-care, coffee and craft, virtual stretching, social Saturdays, art therapy and a psychoeducation group. These continue to operate successfully, with more groups being developed based on consumer needs and feedback.
“I have done more for myself in the past two months than I had in previous years. I feel good that I now have control over my life” – Maeve
Pete’s story
Each day, Pete keeps improving and has been able to achieve his most important goal – seeing his daughter
Pete had a long history of trauma. Recently out of prison, he then stayed in a short stay psychiatric unit after a suicide attempt. Pete had never really been connected to any services along the way and the minimal contact he did have was not a positive experience.
Support Facilitator, Susan from Ermha first met Pete in September 2019. She used a narrative/conversational approach in her assessment to understand Pete’s situation. Susan quickly built a strong rapport with Pete and found he had many goals he wanted to achieve. Pete had a clear direction for what he wanted to achieve for himself and his young daughter, who he had not seen for a few years.
Pete told Susan he often felt unheard and that most people he spoke to judged him. At that stage, he was living in a tent on the beach and was desperately seeking support for his mental wellbeing, so he could see his daughter again.

During Pete’s stay in prison, he was diagnosed with Borderline Personality Disorder (BPD). Susan referred him to a specialist BPD clinic where he has since had psychiatry and psychology assessments and reviews. Peter was also accepted into an ongoing Dialectical Behaviour Therapy (DBT) program.
In addition, Pete was connected to an Alcohol and Other Drugs (AOD) counsellor and was recommended to join a men’s behaviour group – which Pete willingly did on his own.
With the assistance of Ermha, Pete submitted a successful priority housing application and was assisted with the submission of a disability support pension application.
Pete has since been referred to SEMPHN’s Mental Health Integrated Complex Care (MHICC) team where he now receives ongoing mental health support. To provide Pete with further assessments and ongoing psychological care, MHICC, in collaboration with Ermha, successfully applied for funding for an ongoing psychiatrist and neuro-psychological assessment in conjunction with ongoing DBT treatment.
Each day, Pete keeps improving and has been able to achieve his most important goal – seeing his daughter.
For information on PSS and how to access support visit https://www.ermha.org/pss/ or https://www.semphn.org.au/commissioning/mental-health/psychosocial-supports.html
Psychological support for residents in aged care facilities
Evidence suggests mental health problems are under-identified and under-treated by primary healthcare professionals. Some symptoms may be dismissed as part of the ageing process or confused with conditions such as dementia and delirium. In addition, stigma surrounding mental illness makes older people reluctant to seek help.
SEMPHN, in partnership with Better Place and Star Health, is supporting Residential Aged Care Facilities (RACF) to deliver a range of individual and group interventions that are consistent with those available under the Commonwealth Better Access to Mental Health Care program.

In south east Melbourne, there are currently 158 Residential Aged Care Facilities (RACF) with approximately 13,447 residents. Analysis of mental health support within these facilities demonstrated service gaps with a need to have a better framework to support the mental health needs of their residents.
SEMPHN has already invested $4.1 million into providing mental health support to RACFs following the success of its pilot program in Mornington Peninsula, delivered by Better Place Australia. In 2019, SEMPHN commissioned Star Health to expand this service to RACFs across the rest of our region.
RACF Psychological Services offer flexible, brief and goal-directed psychological interventions in RACFS to support residents with a mental illness.
Across the Mornington Peninsula, Better Place is delivering psychological interventions in half of the RACFs (11 of 22) across the Mornington Peninsula. In February this year, Star Health commenced psychological interventions in 22 RACFs across the rest of the region but has been impacted on the expansion of services due to the COVID-19 Pandemic.
Mental health and wellbeing support during COVID-19

COVID-19 has had a significant impact on aged care facilities, not just physically, but mentally, with many residents reporting feeling “worried” and “anxious” for themselves and their loved ones.
Facilities encountered their own challenges. Some were not able to let residents freely visit other units, while others found it hard to engage residents in activities while trying to maintain physical distancing. As restrictions continued, visits from friends and family were not permitted. Many RACF staff noticed residents’ moods flattening and the condition of those with depression starting to decline.
During this time, senior practitioners from Better Place and Star Health were able to support these residents with psycho-education and individual support via telehealth.
Residents who had to self-isolate were able to use telehealth as a way of engaging in their regular sessions and those requiring access to Alcohol and Other Drug (AOD) services were referred to specialist AOD support.
Residents required to remain in their rooms were referred to wellbeing services automatically. Most agreed to receive wellbeing sessions to increase their level of connection and interaction. Many residents reported these sessions having a positive impact , working closely with their practitioner to establish clear therapeutic goals.
Working through grief over the phone
SEMPHN continues to support GriefLine with funding to deliver telephone interventions through their police line service, which has assisted over 1500 consumers referred from Victorian Police for trauma, grief and loss support.
GriefLine is Australia’s only dedicated loss and grief national telephone counselling service. It provides responsive, evidence-based and personalised services for individuals, families and community groups. As part of our Stepped Care Model, it focuses on people in the community who are at risk of mental illness.

Within the last 12 months, GriefLine has undergone significant improvements to its service including:
- Outcome measures are now collected both at the start and end of single sessions (including provision of support over the phone)
- Development of an evidence-based, trauma-informed six session counselling model to support consumers referred by the police line. This model also includes an anniversary follow up with the consumer to check how they are travelling.
- Development of comprehensive downloadable training modules on the GriefLine website.
- Introduction of video consulting as a modality for Police Line consumers (delivered through Cyber Clinic’s online platform, funded by SEMPHN).
- Set up of a new Telephone Support Hub in GriefLine’s central office with the capacity for eight counsellors supervised by two senior clinicians.
- Updated to a more integrated telephone system that supports improved reporting and better facilitates for the coaching of staff and volunteers.
As with other services, GriefLine consumers can ‘step up’ to higher intensity services if required and similarly, higher intensity services can ‘step down’ to GriefLine programs, where appropriate.
Stephen’s story
Throughout all the sessions, the GriefLine counsellor was able to work with Stephen’s feelings of guilt, which has helped him enormously in his journey to recovery
Thirty-year old, Stephen returned home from work one day to find his wife had died from a severe asthma attack. Stephen attempted to perform CPR but was unsuccessful. The couple had a four-year-old child who was home at the time.
As Stephen grieved the loss of his wife, he began to feel highly distressed, confused, guilty and even angry at himself. He felt overwhelmed at the thought of his responsibilities as a sole parent and the implications of having to answer questions from his child.
The couple were originally from New Zealand and did not have any family in Australia. They had made some friends since moving, but often remained quite private, particularly Stephen who only felt comfortable sharing his feelings with his wife.
Stephen was able to connect with GriefLine who dedicated his first three sessions towards his overwhelming grief. In between these sessions, the GriefLine counsellor was also able to send therapeutic SMS messages, which he found very useful in relation to processing his loss, grief and acute trauma.
Throughout all the sessions, the GriefLine counsellor was able to work with Stephen’s feelings of guilt, which has helped him enormously in his journey to recovery.
The sessions with Stephen continued for over three months. Following that, Stephen was able to call the GriefLine counsellor anytime he felt he needed further support.
“In the middle of it all, it was really nice to be able to take some time to focus on how I was going and to realise that I actually really needed to look after myself too” – Stephen
For more information and to access GriefLine visit www.griefline.org.au or call (03) 9935 7400







 Increased Access to Better Mental Health Care
Increased Access to Better Mental Health Care