Reducing harmful impacts from Alcohol and Other Drugs
The impacts of social isolation during the pandemic has shown a significant increase in alcohol and substance misuse across Melbourne’s south east.
Since the COVID-19 pandemic, around one in five adults purchased more alcohol, with the highest consumption in males and females aged 35-44.
SEMPHN acknowledges the priorities of the National Drug Strategy 2017-2026 and aligns our commissioned treatment services to these objectives. We also recognise the services provided via Victorian funding and work collaboratively to reduce service duplication and enhance the system response to the needs of the community.
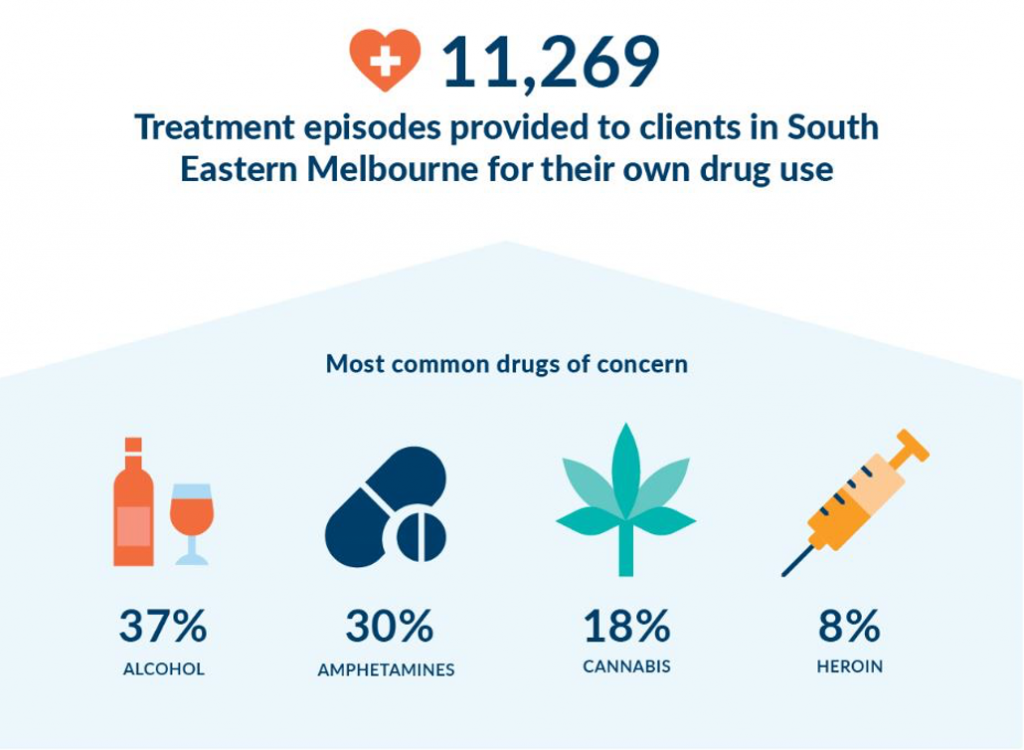
In the last year, SEMPHN invested $4.2M to commission a wide range of Alcohol and Other Drug (AOD) services and activities to support vulnerable Victorians across the region.
Listening to our community
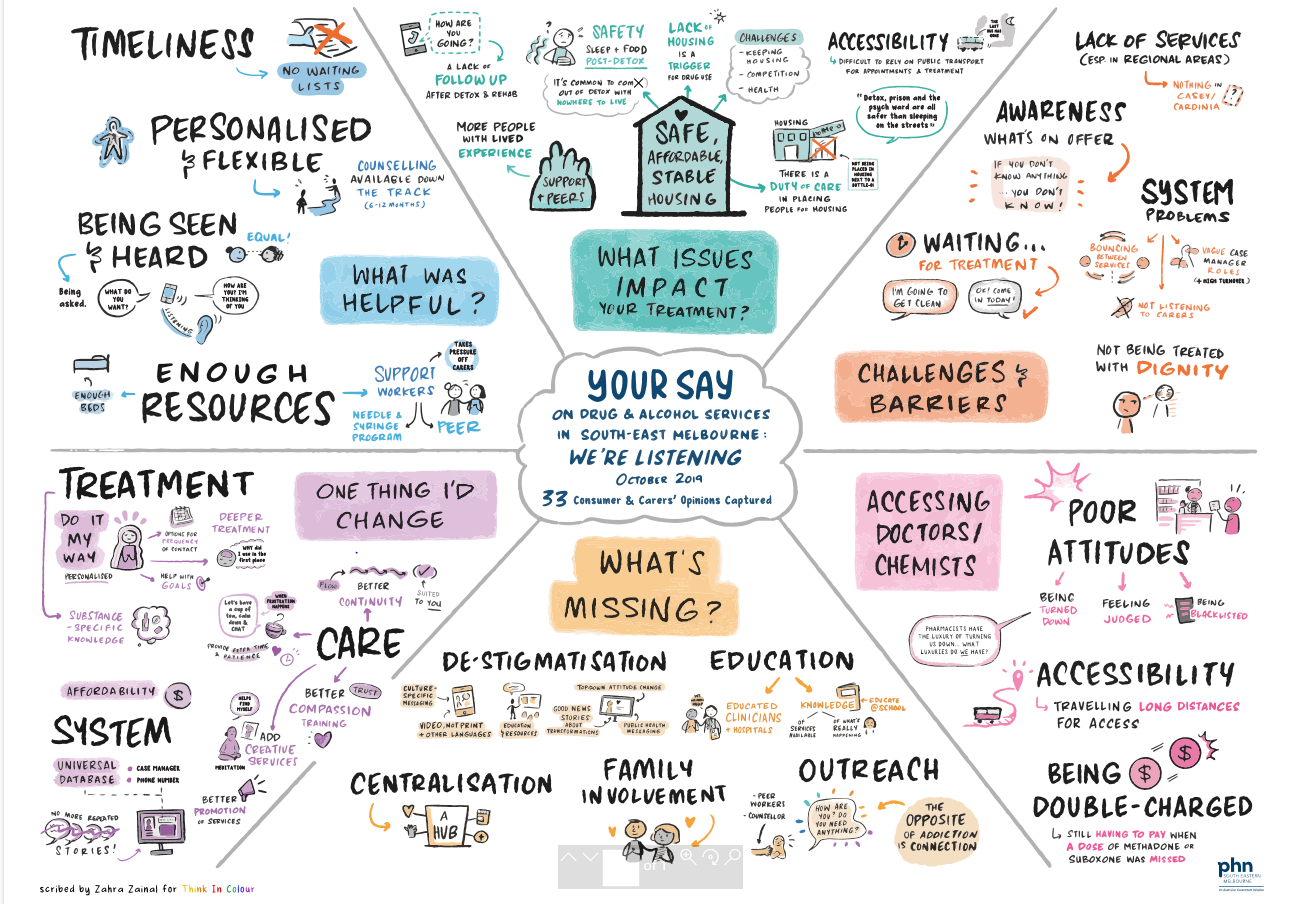
To help inform our planning and decision making, SEMPHN facilitated face-to-face and online consultations with our community which enabled us to identify, learn and understand existing service barriers and challenges for people impacted by alcohol and other drugs.
In October 2019, SEMPHN hosted four face-to-face consumer and carer forums in Frankston, St Kilda, Dandenong and Narre Warren. The results were used to help identify the current needs within the south east catchment and to help inform future commissioning plans for AOD services.
Here is what the community told us about the improvements they wanted to see
• No waitlists, more rehab beds
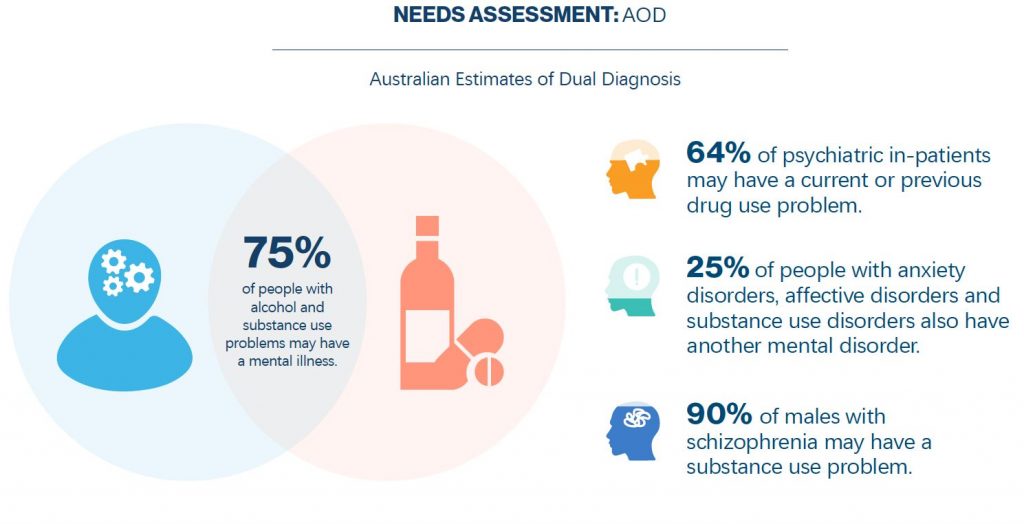
• Improved continuity of care, including for patients navigating AOD and mental health services
• Empathetic, more highly skilled AOD workforce
• Simplify every aspect of the AOD treatment journey
• Better promotion of services for consumers, carers and their families
• More cost-effective rehabilitation services that continue to provide ongoing care
The collated consumer and carer feedback [see diagram] is an invaluable resource for the development and improvement of appropriate SEMPHN-commissioned services in the future.
Thanks to the Association of Participating Service Users for their support in coordinating and facilitating these sessions.
Jade’s story
Jade is a 34-year-old mum from Frankston who has a complex relationship with prescription and illicit drugs. She experiences the challenges of unstable housing and believes she has Borderline Personality Disorder but is waiting on a formal diagnosis. Jade is well connected to health and community services but lacks support from friends or family.
Nicholas’ story
Nicholas is a 48-year-old man from St Kilda who has gone through several periods of being homeless. Nicholas has been unemployed for a long time and has no support from family or friends. He is currently seeing a psychologist for Post-Traumatic Stress Disorder (PTSD) and has challenges with substance mis-use gambling, but feels he needs better support. He is finding it hard to change his ways.
Taking the first steps to recovery
We work with our partners and the sector to ensure that evidence-based treatment and services are easily accessed by those experiencing risky levels of AOD use.
In 2019, SEMPHN commissioned First Step to deliver ResetLife, an evidence-based AOD treatment program using the Matrix Treatment Model in the local government area of Port Phillip.
This program was first established in Frankston to help tackle harm caused by alcohol and drug use, as part of an Australian Government National Ice Action Strategy funding package for AOD services across south Eastern Melbourne.
ResetLife is an alternative and/or complementary treatment type to residential rehabilitation. It allows people with AOD dependence to stay at home while they access intensive outpatient rehabilitation treatment.
During the COVID-19 pandemic, through consultation with SEMPHN, First Step moved to an online platform to ensure new clients were able to access the program. First Step also created an informal online support group for ResetLife clients and paid for additional internet data where cost may have been a barrier for clients’ participation.

Reuben’s journey
Thirty-four-year-old Caulfield resident, Reuben endured a long struggle with cannabis addiction for 15 years, which significantly impacted his mental wellbeing and daily activities.
“I remember being at the Alfred Hospital and feeling vulnerable when the doctor came in and suggested I reach out to First Step as part of my discharge. I knew I needed the help, so I gave them a call.
After my hospital stay, I began the program where I was connected to therapists who were very empathetic, warm, and highly equipped to support me on my journey. The emphasis on keeping a schedule was new to me, yet it helped me immensely. The weekly meetings included topics such as, “How to deal with guilt and shame,” and “Motivation for recovery and getting on top of finances.”
The education I have received has been integral to where I am now. There have been highs and lows throughout the program, but not once did I think I couldn’t push through. I had the tools and the psychological explanation to make sense of what I was experiencing. Finally, in spite of previous unsuccessful interventions, I knew I was equipped to overcome the obstacles in front of me.
I have resolved all my debt and have started managing my money for the first time in my life. I am so grateful to have my life back, to feel like myself again and most importantly, to be able to reconnect with my family”.
“I am so grateful to have my life back, to feel like myself again and most importantly, to be able to reconnect with my family”
Find out more about ResetLife and how to access support
Support for women and their families

We are committed to providing mothers who are experiencing dependence on alcohol and/or other drugs with access to intervention while ensuring intensive support is also available for their children and significant others.
Evidence shows that well-coordinated and comprehensive support with early access to care and specialist AOD treatment can reduce harm and improve outcomes for women who have problematic alcohol and drug use – and their families.
SEMPHN commissioned Taskforce to deliver Breaking the Barriers, a parenting support program for families designed to reduce substance use while improving individuals’ health, wellbeing and social connectedness.
A key focus of this program is to identify, address and reduce the harms associated with comorbidity issues (for example, mental and physical health, AOD, homelessness, family violence) that may be associated with the individual and their family.
Taskforce has been able to continue delivering services during COVID-19 via virtual meetings with new and existing clients.
Sarah’s journey

Sarah had a long history with substance use and had just given birth to twin girls. She already had two boys with special needs and was still grieving the loss of her mother. Her partner required open heart surgery, which put financial stress on their one-income family and required them to move to a new house shortly after Sarah gave birth.
“Sarah’s mental health is now more stable. She reports not using marijuana for five-weeks and reducing her alcohol consumption to weekends only”
Sarah was referred to the Breaking the Barriers program by the maternity team at the hospital. At first, she was reluctant to accept support, so it took time to build rapport and trust. During this time, the program offered practical and flexible support to help Sarah. This included financial support to help Sarah buy groceries, as well as uniforms and school supplies for her sons. The program also helped Sarah to secure childcare for the twins so she could have a regular break.
After some time, Sarah’s mental health improved. Her psychotic symptoms dissipated, enabling her to cease her medication with the support of her doctor. Her engagement with the program improved, which was an important foundation for the additional challenges posed by COVID-19, which impacted her income and put additional pressures on household. The program continued to support Sarah during this time by connecting her to appropriate financial supports, food relief and counselling.
Sarah’s mental health is now more stable. She reports not using marijuana for five-weeks and reducing her alcohol consumption to weekends only. The family has achieved significant outcomes, with Sarah continuing to participate in case management through telehealth services.
For information on how to access Breaking the Barriers visit www.taskforce.org.au/adult/
Improving access to treatment
Ensuring vulnerable individuals have access to appropriate care is vital to reducing harm caused by alcohol or other drugs and minimising the impact on individuals and their loved ones.
Over the last year, one in four of Australians reported consuming alcohol at risky levels on a single occasion and around one in five Australians exceeded lifetime risk guidelines. Around 3.4 million people reported illicit drug use.
The Alcohol and Other Drug Liaison Outreach Workers (ADLOW) program was established to improve service access and treatment options for drug use in the cities of Port Phillip and Greater Dandenong. Now in its third year, SEMPHN funds a support worker to provide an in-reach service to hospitals across the region to help young people and adults connect to community alcohol and drug services.
Within the last 12 months, over 250 people were referred to the program which provided these clients with brief interventions, counselling, withdrawal management, pharmacotherapy support, care coordination and referrals to other appropriate services.
Renee’s journey
“The ADLOW clinician was there every step of the way to support Renee as she recovered from her mental ill-health and gradually ceased her use of methadone and cannabis”

Forty-seven-year-old Renee was a regular cannabis user and had a history of injecting heroin. At the time of referral into the ADLOW program, she was on methadone replacement and was experiencing episodes of paranoia. Renee’s goal was to cease her methadone with a longer-term goal to attend residential rehabilitation for her cannabis use.
While her mental health was the initial priority, Renee was able to focus on her treatment for substance use after a few appointments. The ADLOW clinician was there every step of the way to support Renee as she recovered from her mental ill-health and gradually ceased her use of methadone and cannabis. Her doctor’s appointments focused on providing harm minimisation strategies. Renee was then referred to an appropriate residential rehabilitation, and AOD Care and Recovery Coordination at TaskForce.
The coordinator is assisting in Renee’s treatment and providing individualised and flexible support while she waits to hear the outcome of her referral to residential rehabilitation.
To find out more about accessing ADLOW visit https://taskforce.org.au/wp-content/uploads/ADLOW-flyer.pdf







 Reducing Harmful Impacts from Alcohol and Other Drugs
Reducing Harmful Impacts from Alcohol and Other Drugs

