Working towards a healthier community
Chronic diseases are the leading cause of illness, disability and death in Australia with 76 per cent of the south east population identified as high-risk due to their lifestyle choices.
Managing chronic disease has steadily become a large part of general practice workloads. However, primary health systems and frameworks are often not structured to provide a best-practice response to chronic disease management.
SEMPHN is continuing to work with general practices and other partners to improve chronic disease management through a range of commissioned programs aimed at preventing and managing chronic health conditions across the region.

12% of people (18 yrs+) experience high or very high psychological distress
53% of people with inadequate fruit or vegetable consumption
15% of people more than two standard alcoholic drinks per day on average
24% of people have high blood pressure
64% of people undertake no or low exercise
76% of people have one of four risk factors (current smokers, high risk alcohol, obese, no or low exercise in the previous week)
Connecting young people to appropriate care
There are over 4,000 children in Out-Of-Home-Care (OOHC) settings in Victoria. This which includes around100 children and young people living in residential care in south east Melbourne.
SEMPHN, in partnership with general practices, is supporting OOHC by providing localised access to medical services, including mental health.
Young people in residential care are some of the most vulnerable members of the community. Their level of severe trauma (neglect, sexual abuse, physical abuse) is disproportionately higher and they often have further complications such as substance mis-use and a series of special (and often unmet) needs.

OOHC is designed to strengthen person-centred care, particularly for people living with complex and chronic health conditions and to improve the health and wellbeing of vulnerable children and young people in Victoria. General practice plays an important role in preventing, diagnosing and addressing the range of physical, neurological, developmental, psychological and behavioural issues that present in many children and young people in these settings.
SEMPHN works with local practices to, enable residents to access more medical services, including mental health, when they most need it.
Within its first year, 170 appointments were made with three quarters of young people accessing the services for a range of referrals identified during GP consultation, such as optometry, psychology, audiology, paediatrics, dentist, physiotherapist and dietitian.
A key success has been sustainability, with general practices across the south east continuing to support residential homes beyond the funding of the program.
Tuberculosis screening, management and prevention in general practice
In Victoria, an estimated 300,000 people have Latent Tuberculosis Infection (LTBI). It more commonly affects those born in TB-endemic countries. Data suggests that around 17 per cent of those born overseas live with LTBI.
While Tuberculosis (TB) is an uncommon disease in Victoria, it continues to have a significant impact on affected individuals and families. The risk of transmission, and the length of time that TB persists for, means beyond the physical effect of the disease and treatment, many people experience financial difficulties related long illness, interrupted work and studies, and provision of care for family members.
Unfortunately, TB is a condition which still has associated stigma in many communities, which can lead to social and psychological harm for those affected.
As trusted care providers, GPs play an important part in the diagnosis and management of LTBI in the community, and early access to medical treatment is imperative.
The SEMPHN Tuberculosis Screening, Management and Prevention Project was developed to pilot a general practice education and support program for LTBI management.
In partnership with the Victorian Tuberculosis Program team at the Peter Doherty Institute for Infection and Immunity, we conducted a pilot project aimed at further educating and supporting general practices to manage LTBI safely and effectively within a primary care setting.
The pilot focused on the development of resources and specific TB training for general practice staff, to build enhanced capacity and confidence of practices to screen, test and treat LTBI.
Evaluation of this pilot highlighted that a multifaceted and prevention-focused approach to communicable disease is effective. The program resulted in 10 patients who completed treatment for confirmed LTBI and 16 who remained in active treatment.
Understanding and treating Tuberculosis in primary care
When Associate Professor Justin Denholm from the Victorian Tuberculosis Program first established this project, he envisaged that it would primarily help general practitioners to provide LTBI treatment to their own patients, rather than to refer them to hospitals. While that would have been a great benefit, Associate Professor Denholm has been delighted to see additional opportunities arise as the program evolves.
Having developed the skills to diagnose and treat LTBI safely, one of our participating clinics established a partnership with a migrant screening service to support people found to have LTBI and who were unable to access ongoing care.
This innovative connection helped them to provide patients with a local service that they may have otherwise missed and is a great example of patient-centred health.

Associate Professor Justin Denholm (pictured front-left with his team) is the Medical Director of the Victorian Tuberculosis Program. He is a Senior Staff Specialist at the Victorian Infectious Diseases Service at the Royal Melbourne Hospital, and Principal Research Fellow in the Department of Microbiology and Immunology at the University of Melbourne.
Improving care for people with chronic and complex needs
Caring for our community is becoming more complex with an ageing population and increasing incidence of chronic disease. Many people are living with more than one chronic health condition, requiring access to multiple services to manage their care.
In partnership with general practices, SEMPHN is improving care for patients with chronic and complex needs by supporting the timely coordination of health, community and social services.
In 2019-20, there were an estimated 1,260 people per 100,000 hospitalised for potentially preventable chronic disease. Many also experienced barriers to accessing support services in their area.

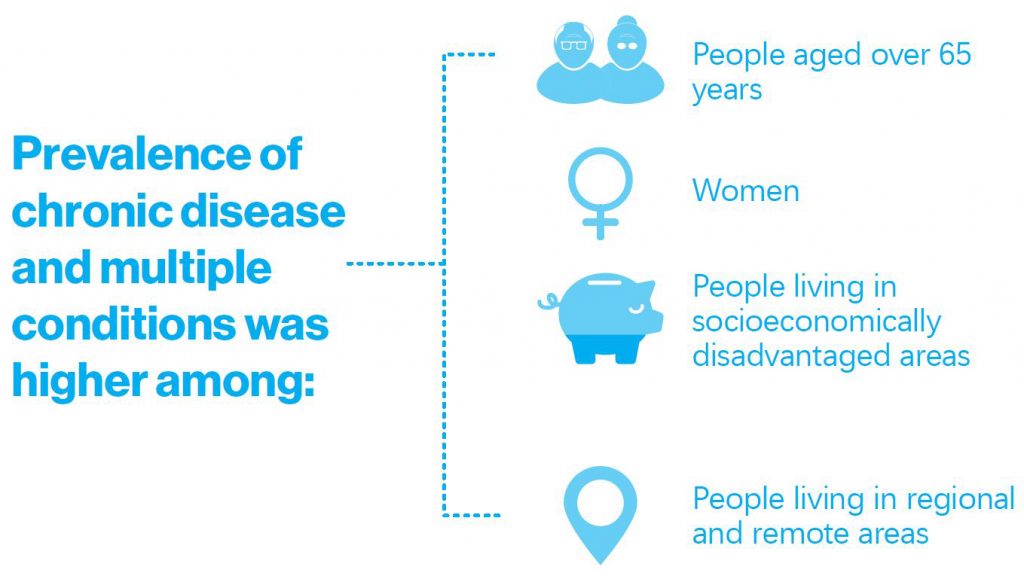
Prevalence of chronic disease and multiple conditions was higher among people aged over 65 years who are:
- Women
- People living in socioeconomically disadvantaged areas
- People living in regional and remote areas
In 2019-20, SEMPHN committed $6.5 million towards the delivery of coordinated care for patients with a chronic disease condition(s) or complex needs.
Twenty-eight general practices across the south east received funding through SEMPHN’s care coordination program. The commissioning piece was developed to further build capacity in general practice and to support the comprehensive care of patients who live with a chronic disease.
Since last year, the program has had over 2,800 patients enrol with around 900 patients receiving 12 months of care coordination.
Key highlights
- 448 refugee patients accessed care coordination through 11 general practices
- 100% of practices developed new Chronic Disease Care Plan templates that include After Hours medical care options for patients
- 83% of patients have an action plan for their chronic condition’s acute health needs
Connecting and coordinating culturally appropriate care
Barb’s story
Barb is a local 70-year-old woman who identifies as Aboriginal Torres Strait Islander. She has multiple health conditions including an intellectual disability and requires ongoing treatment for pain. Without adequate family support, Barb has not maintained her regular appointments, often requiring Casey Medical Centre to follow up and check in on Barb’s wellbeing.
SEMPHN’s care coordination program has enabled Casey Medical Centre to connect Barb to culturally appropriate support services including regular outpatient appointments at Dandenong and Monash Hospitals. Under the program, Barb was supplied with taxi vouchers to assist in travelling to the hospitals, where she was greeted by a support facilitator who accompanied her to her appointments. The care coordination program continues to provide valuable support for Barb to ensure her physical and mental health needs are being met.

National Bowel Cancer Screening Project
SEMPHN, in partnership with Cancer Council Victoria, has been engaging the community through various activities to promote the importance of bowel cancer screening and increase screening participation.
The success of this program saw almost 5,000 extra bowel screening kits analysed within the first six months. 1 in 13 people are diagnosed with bowel cancer and if detected early, 90 per cent of people make a full recovery.
Bowel cancer screening rates remain low across the catchment. Less than 40 per cent of people over 50 were screened for bowel cancer, making our region the second lowest for bowel screening participation in Victoria.
SEMPHN commissioned Cancer Council Victoria (CCV) – in a 2.5-year project – to deliver the National Bowel Cancer Screening Program (NBCSP) across the region with the aim of increasing participation rates by an additional 7,000 screens over what would normally be expected.
In addition, SEMPHN and CCV engaged Professor Jon Emery from the University of Melbourne to support the academic component of this project, providing valuable research updates and information to GPs, practice managers and nurses in the region. Almost 300 practice staff undertook academic detailing sessions specifically designed to help increase their knowledge about the NBCSP and how to best support their patients. Academic detailing in this program involved peer-to-peer educational support offered from experienced cancer council nurses at CCV to primary healthcare professionals in primary care. During COVID-19, an online training module was developed for general practice staff in the region as an alternative to the face-to-face academic detailing sessions.
Academic detailing is “university or non-commercial-based educational outreach.” The process involves face-to-face education of prescribers by trained health care professionals, typically pharmacists, physicians, or nurses.
Reaching vulnerable and Culturally and Linguistically Diverse (CALD) communities remained a focus throughout the project. Community resources, activities and information sessions were delivered to meet cultural needs. Since the project commenced, a total of 177 community members attended community engagement sessions in Springvale, Dandenong, Doveton and Frankston. Community members included Vietnamese, Arabic and Tamil speakers and members of the local Aboriginal and/or Torres Strait Islander community.
Key highlights
- In 2019-20, in the first six months of the project, the NBCSP analysed almost 5,000 extra bowel screening kits from the region
- 125 academic detailing visits were undertaken across general practices in the region
- More than 16,500 people were reached with bowel screening messaging through geo-targeted social media advertising







 Working Towards a Healthier Community
Working Towards a Healthier Community